Searching for the anchor value and reaching the turning point
James Fleck: Anticancerweb 09 (03), 2019
Practice of Multidimensional Integrative Medicine begins with a professional attitude responsive to the patient's needs and rights. Proper professional behavior promotes empathy, which is a human feeling that cannot be imposed. It should be achieved and maintained through a very qualified doctor-patient relationship. Developing empathy is a personalized work, not admitting a preprogrammed approach to modulate human behavior. The physician, exercising his sensitivity, seeks the dominant behavior trait of each patient, which is called anchor value.
There is a high specificity in expressing the anchor value.
Based on Schwartz's international research, at least ten major human values were recognized worldwide. However, there was great heterogeneity in the priority profile of human values.
Today, increasing world population further stimulates diversity. Political, social and even humanitarian efforts are systematically failing to identify a comprehensive set of human values. Despite the growing communication resources, media are essentially driven by consumer society, creating stereotypes. Internet reinforces people connection, but also stimulates an illusory idea of an individual egocentric position in the universe. Currently, a large number of biopsychosocial components are responsible for stratification of human values. Only a multidimensional system, possibly supported by big data analysis, could eventually better categorize human values. However, this is still fictional.
Patient-physician relationship should rely on art.
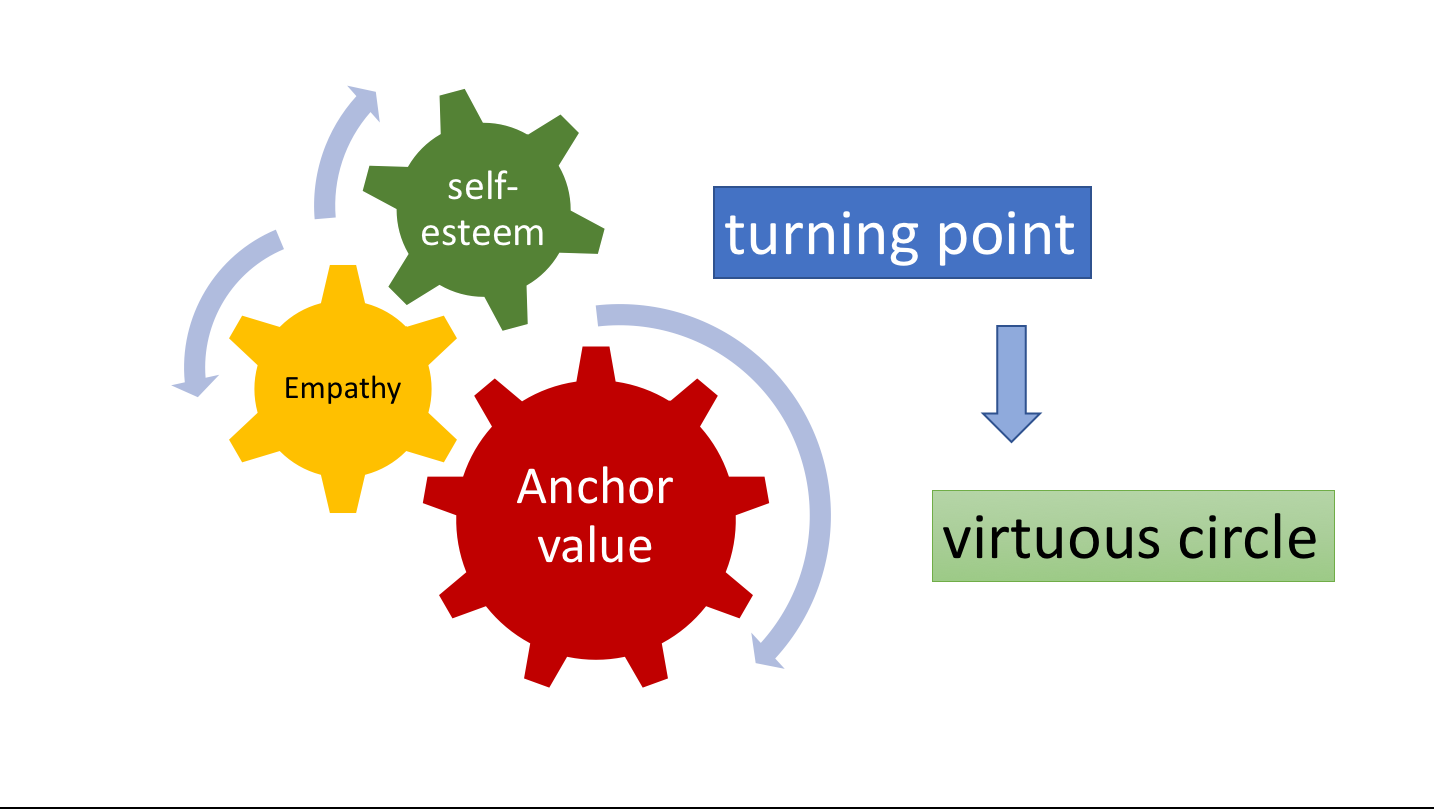
Identification of patient’s anchor value should be supported by physician’s sensibility. Facing crises, patients better express feelings, opening a true-line of communication. Anchor value usually reflects the strongest motivation on life. Empathy results from the ability of the physician to identify patient’s anchor value. Empathy favors patient's randomly aggregation of other human values, creating a virtuous circle. Physician, assuming a coaching approach, promotes recovery of patient’s self-esteem, leading to the turning point.
Ideally, patient’s turning point should precede physician's recommendation. Following the turning point there is a decrease in the emotional flow, making patient more attentive and prone to better understand the intervention. Timing for patient’s self-esteem recovery is also proportional to the degree of mutual confidence achieved through patient-physician relationship. Based on empathy it is also possible to initiate a patient educational program. Patient should understand how physicians think and how they support their recommendations. Cognitive psychology resources further stimulates patient’s protagonism. Patient spontaneous searching for knowledge is well-received. However, doubts are better clarified through a direct interface with the physician. Reasoning is gradually integrated into the art-oriented virtuous circle, better qualifying shared decision-making.
References:
Schwartz S: Universal in the content and structure of values: Theoretical advances and empirical tests in 20 Countries, Adv Exp. Social Psych25, 1992
Schwartz S, Cieciuch J, Vecchione M, et al: Refining the theory of basic individual values, Journal of Personality and Social Psychology 103: 663-688, 2012

As medicians, we have to consider that a life isn’t restricted to its biological behaviour. People have differing interests and concerns and all of that influences the way of dealing with health, process of disease and healing. In that way, one great method to construct a reliable connection with patients is through art. Capable of interfering with the individual’s deepest form of sensitivity, all forms of art can turn into a bigger motivation to live. At the hospital, for example, paintings all over the walls, letters of preceding patients, reading groups and writing workshops can alleviate patients’ pain, incomprehension, mourning process and other hard feelings.
While I was reading this, a book written by Viktor Frankl came to my mind. In this book, called “Psychotherapy and Meaning of Life”, the author did not try to reasure his own values through his theory, instead he reinforced the idea that the core principles that guide each person’s life are unique, even though there are shared values among the community - and even different cultures. I believe this goes along with the article, given that it proposes an individualized relationship with the patient, caring for what’s most important to them, without trying to impose our own values to them. This is an imperative when it comes to empathy, which, in turn, is essencial for quality care.
While I was reading this, a book written by Viktor Frankl came to my mind. In this book, called “Psychotherapy and Meaning of Life”, the author did not try to reasure his own values through his theory, instead he reinforced the idea that the core principles that guide each person’s life are unique, even though there are shared values among the community - and even different cultures. I believe this goes along with the article, given that it proposes an individualized relationship with the patient, caring for what’s most important to them, without imposing our own values to them.
Building a qualified patient-physician relationship is indeed a challenging process. On one hand, the patient, with no doubt, wants to be able to trust his doctor and to be understood by him during the difficult situation which is facing a disease. On the other hand, the physician, although willing to diagnose and treat the patient, usually doesn't pay attention to what's going on beyond the organic disease. Besides, sadly an always overwhelmed physician is still seen as normal, especially inside the medical community. Because of that a lot of doctors think that their lack of meaningful relationships with patients is justified by the following reasoning: physicians have too many patients and too little time to see all of them, so it's expected and even obvious that the relationship with patients will be superficial. Actually this reasoning is a fallacy but unfortunately just a few doctors have already realized that. So, physicians as a whole need to recognize that a trustful patient-physician relationship can improve patient adherence to treatment, encourage the patient to always be honest and make the patient feel comfortable while discussing his fears and expectations during medical appointments. One way to start creating a qualified relationship with patients is, as exposed in this editorial, trying to figure what is the anchor value of the patient. When that's figured out the physician can be truly empathetic with each particular patient and then finally make the patient feel safe and invited to be part of a shared decision making relationship.
Please login to write your comment.
If you do not have an account at Anticancerweb Portal, register now.