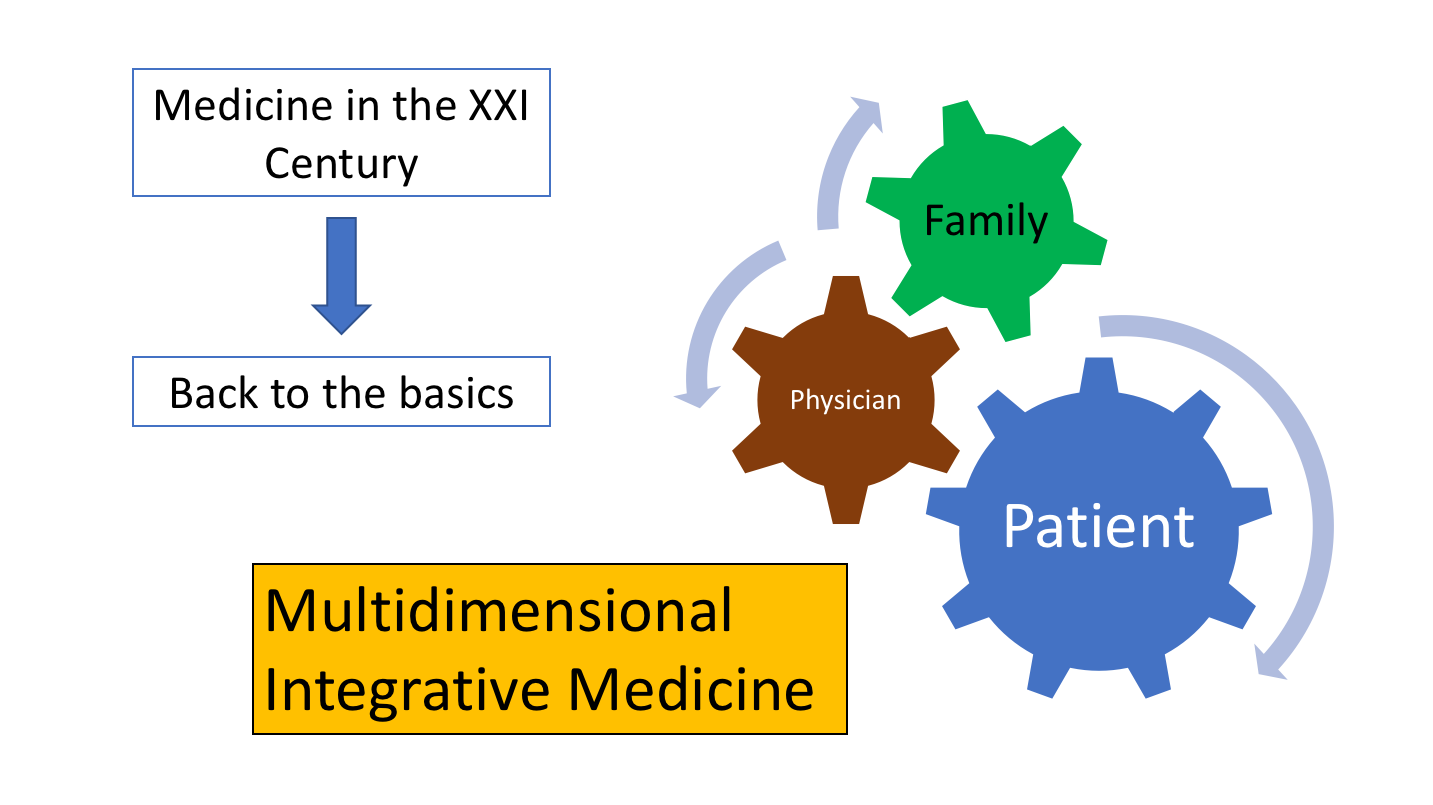
Back to the basics
James Fleck: Anticancerweb 3(03), 2019
Practice of Medicine is essentially centered on patient-physician’s relationship. All medical interventions are supported by levels of evidence and must be proposed based on patients' needs and rights. Patient should clearly understand the recommendation and physician should guide him or her on a shared decision-making. Routine use of the therapeutic index, encompasses risks and benefits. Recommendation should rely on well-defined epidemiological criteria (NNT and NNH), leading to the best cost-effectiveness ratio. Many medical interventions are dictated by algorithms and classified by a predefined grade of recommendation. An excellent example in clinical oncology is the National Comprehensive Cancer Network (NCCN)1, which has been orienting physician’s recommendation for more than 20 years.
Physician's recommendation has to be fully understood by the patient and patient's compliance should always be preceded by a written informed consent.Multidimensional vision of Medicine broadly reaches all these goals by integrating functional, emotional, cognitive and social components in a sharing decision-making.
Multidimensional Integrative Medicine requires some sequential modeling interventions. The first intervention is directed to the staff, consisting of the removal of self-protection artifacts. Symbolic elements used to reinforce physician's self-image should be abolished. They are usually aversive to the patient. The white gown should be discharged. It only imposes an undesirable sense of authority, resembling a military uniform. Unconsciously, it creates a disproportional and conflicting impression between a weak and illness person and a rigid well-dressed physician’s stereotype. The physician should enter the room disarmed, with no computer, tablet, phone, chart, pen or even patient’s exams. He should sit and listen to the patient, with serenity and genuine empathy. He should encourage the patient to talk about own life and the impact the disease is producing in daily activities, work and family relationships. This attitude requires only a few minutes, but is extremely important to create patient’s sense of belongingness, moving toward an integrative behavior. Belongingness is additionally stimulated by changes in the office environment. Design should abolish any kind of desk. The presence of a desk obstructs the body language, favouring a formal and awkward attitude. Physician's chair should not be different from that used by the patient. Preferably, a circular meeting format should be adopted, where physician, patient and family would talk freely.
In the office room there is no assigned chair. Patient and family are free to choose where they want to sit and the physician should take the vacant place. The heights of the seats should be equal, favoring eye contact. Office design would resemble a living room. Decoration should be clean, with images pointing to life and nature, preferably with natural lightening. Belongingness has always been central in conducting human relationships. Since the beginning, mankind was organized in social groups, not only to survive but also and specially to share experiences. Social bonds promotes collective consciousness, which improves self-esteem and a positive attitude toward overcome disease and suffering. Belongingness favorably modifies the self, moving him or her toward auto-realization, altruism and transcendence. Later on, physical exam is performed in another room, contemplating patient’s privacy. Diagnostic tests, when available, are uniformly discussed after physical exam when an interpersonal trust has been achieved. The recommendation will be an integrative result of all previous steps, occurring at a time when patient is already confident, fully exercising his/her competence for a shared decision-making.
NNT = Number Needed to Treat
NNH = Number Needed to Harm
Reference:
National Comprehensive Cancer Network (NCCN) ( www.nccn.org), 2018

An image of the “all-powerful” doctor is not compatible with what is recommended as major medical societies. Those doctors who have not yet taken on a multidimensional view of the patient, with their functional, emotional, cognitive and social characteristics, miss the opportunity to treat the patient as a whole, as a single person. Based on a family experience, I believe that the oncologist, especially, needs to be like this due to the emotional complexity in which the patient reaches him. In the words of a my family member who suffers from non-small cell lung cancer, “the best doctor is not one who knows everything, but one who listens to the patient”. It is good to know that medicine is taking this path.
I had never really thought about how the interior design of a doctor office could impact the sucess of the bonding with the patient. Certainly I’ll take this in account when I become a doctor. Now that I’m a medical student, I think about the frustrated medical appointments I already had in my life, and got to the conclusion that what was missing in all of them was a good patient-physician’s relationship. This should be the core of a good medicine pratice, which I'll always seek. “The good physician treats the disease; the great physician treats the patient who has the disease”.
I think we should do everything to try to create a bond with the patient, whether it be changing the office layout, or trying to organize something closer to that at the bedside. I believe that this will help the patient to do better monitoring, feel more secure, and have greater adherence. However, I am very concerned about doctors who have a lot of empathy, but not so much evidence-based knowledge.
As a medical student, I understand that knowing what's going on inside the patient's head is just as important as knowing technical information about the rest of their bodies. That's why I take time in my everyday life to focus on literature about non medical stuff: to be trully related to the most variable social and personal situations and improve my comprehension about every patient.
Please login to write your comment.
If you do not have an account at Anticancerweb Portal, register now.